
Monday March 15, 2021
By Faiza Mahamud and Michael Corey
Through aggressive testing and stringent measures to curb the disease, the city has consistently lower rates of infection and deaths.

Kayse Abdirahman administered COVID vaccine at a pop-up clinic in the Brian Coyle Community Center on Friday. ELIZABETH FLORES
The first surge of coronavirus cases in Minneapolis struck hardest in the Cedar-Riverside neighborhood, where the mysterious virus last April was killing elderly East African immigrants nearly every day.
Public health officials were learning of COVID-19 spreading rapidly in the high-rise Riverside Plaza apartment complex, where riding elevators and carpooling to work at the Amazon warehouse made social distancing impossible.
"We were seeing daily increases in the double digits in terms of the number of cases," said Luisa Pessoa-Brandão, the city's lead epidemiologist. "It was concerning to see that happening and that was a neighborhood that very much was accounting for a large proportion of the cases in Minneapolis."
Now almost a year since the coronavirus crisis, Minneapolis has turned the situation around. Through aggressive testing and stringent measures to curb the disease, the city has consistently lower rates of infection and deaths than many places in greater Minnesota.
An early hotspot is now beating the curve
The Cedar-Riverside neighborhood of Minneapolis was an early epicenter of COVID-19 cases and deaths. But since late summer, Cedar-Riverside's ZIP code has usually reported fewer weekly cases per 1,000 people than Minneapolis or Minnesota as a whole.
The Cedar-Riverside neighborhood, home to a sizable East African community, generally had lower case rates than many Minneapolis neighborhoods in recent months.
Since the pandemic started, the city has recorded more than 33,360 confirmed cases and at least 396 deaths, according to data kept by the city. People of color account for 42% of those fatalities and make up 40% of the city's population. As of last week, Minneapolis had a 20% lower COVID-19 death rate than the state overall.
Minneapolis singled out
Last spring, the situation in the city was dire. In May, the White House coronavirus task force singled out Minneapolis, along with Washington, D.C., Baltimore and Chicago, as the four metro areas where COVID-19 infection rates were persistent or rising.
Health officials, who at the time didn't know much about the disease, quickly identified Cedar-Riverside as a coronavirus hot spot and launched the city's first community testing event in the neighborhood to begin contact tracing and other targeted efforts to stem the spread of the virus.
After other efforts began in Cedar-Riverside, the city's public health officials turned their attention to other neighborhoods, like Phillips and Ventura Village, where the virus was spreading. They partnered with the Minneapolis Public Housing Authority and tapped community members to volunteer at testing centers to ease residents' mistrust of government.
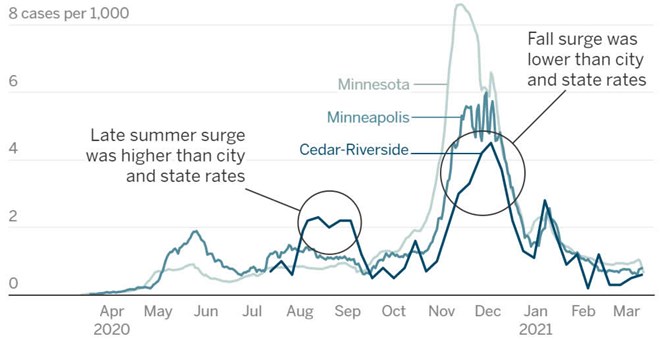
Minnesota and Minneapolis data is released daily. Data for Cedar-Riverside's ZIP code 55454 is released weekly, but was unavailable prior to July.
By C.J. Sinner and Michael Corey, Star Tribune Source: Minnesota Department of Health, City of Minneapolis, 2019 American Community Survey 5-year population estimates.
On May 26, the city enacted a mask mandate before the state made it a requirement. And when unrest erupted in the streets of Minneapolis after the death of George Floyd, city staff who worried protests would set off a spike in infections passed out free masks and hand sanitizer at demonstrations.
According to the city, protests and the riots that followed Floyd's death did not lead to a surge in COVID-19 cases. Case rates in Minneapolis declined from late May through mid-July.
"People were wearing masks, people were trying to maintain some distance, making sure that they were safe because no one wanted to add to the tragedy that already happened," Pessoa-Brandão said.
That stall in the virus' spread allowed the city to brainstorm other ways to break the chain of transmission. City officials expanded testing and Mayor Jacob Frey signed an emergency regulation in July, ordering businesses such as bars and restaurants to shut their doors to indoor services, preventing people from congregating.
Some Minneapolis neighborhoods, including Cedar-Riverside, saw an uptick in cases in August, which epidemiologists attributed to college students failing to social distance. But since September, Cedar-Riverside cases have been on the low end of Minneapolis ZIP codes. Minneapolis health officials credit stringent measures, aggressive efforts and building trust with the community for controlling the spread of the deadly disease.
Dr. John Hick, an emergency physician at Hennepin Healthcare who helped coordinate the state's response to the pandemic, said the number of COVID patients in intensive care statewide is lower than it has been since April when the upswing in infections began. Mask-wearing and social distancing, he said, has helped slow virus transmission, but things are not in the clear yet.
Because of the decline in COVID-19 cases and hospitalizations in Minneapolis, Frey has eased restrictions on city establishments, putting them in line with the state.
Community clinics respond
When the virus ravaged low-income and communities of color this summer, many health centers in Minneapolis had to change their approach. They rolled out robust testing, conducted aggressive outreach and offered COVID resources in several languages.
Some clinics hurried to set up mobile testing in public housing high-rises and other densely populated areas of the city where physical distancing was difficult. They passed out free masks and connected remotely with patients wary of in-person care.
Jonathan Watson, chief executive at the Minnesota Association of Community Health Centers, which represents 17 nonprofit safety-net clinics, said they have tested at least 40,000 people in the past year. The test positivity rate is 17%, significantly higher than the statewide average but roughly half what it was three or four months ago, he said.
Positivity rates of the Minneapolis community health centers have decreased over time even with continued testing, but COVID-19 is still disproportionately affecting people of color, he said.
"It was absolutely crazy," Watson said. "And so, it was just aggressive testing and really getting out to the community to meet them where they're at."
In the last week of April, the People's Center clinic in Cedar-Riverside set up a drive-through, no-appointment testing site. By July when cases spiked, many in the community flocked to the drive-through testing site, including some who had no symptoms but had lost close family members to the disease.
Abdullahi Salad was among those getting tested. Salad, owner of two businesses in Cedar-Riverside, tested positive for COVID-19 in April. Between May and November, Salad lost nine family members to the disease. At least six of his regular customers also died of the disease.
"2020 was one of the most painful and scariest times in my life," Salad said. "I'm still recovering from that trauma."
The community's knowledge of the virus, he said, has changed drastically. Salad said people are now taking COVID seriously.
"It's nobody's fault in the community that we became a hot spot," Salad said. "We weren't getting the state government's early COVID warnings in a language many of our members understand."
Since April, the People's Center clinic has conducted more than 10,000 tests. The number of cases coming back positive has dramatically decreased from the heightened months of July, August and September when the clinic had high rates of positivity among its Black population.
"Many of our families here who live in the Cedar-Riverside area live in multigenerational houses," said Ann Rogers, CEO of the People's Center Clinics & Services. "So, when you're living in a small setting, we also know that the spread of the COVID virus can take place and latch on much, much easier."
On a recent afternoon, the first floor of the People's Center Clinic offered a glimmer of hope to a community that has suffered most from the pandemic. Clinic staff had just wrapped up a long afternoon of testing, an Ethiopian woman danced as she got her first shot of vaccine while elderly Somalis encouraged one another as they waited for their first dose.